Vitamin B12 plays a crucial role in maintaining overall health, contributing to red blood cell formation, neurological function, and DNA synthesis. However, individuals with gastrointestinal disorders may face challenges in absorbing this essential vitamin, leading to potential health complications. In this article, we will explore the intricate relationship between Vitamin B12 and gastrointestinal disorders, shedding light on considerations for absorption.
Vitamin B12, also known as cobalamin, is a water-soluble vitamin found in various animal products. It is essential for several physiological processes, including the production of red blood cells and the maintenance of a healthy nervous system. Dairy products, meat, and fish are excellent sources of vitamin B12. The recommended daily intake varies by age and sex, with deficiency symptoms ranging from fatigue and weakness to neurological issues.
Several gastrointestinal disorders can impact the absorption of vitamin B12. Conditions such as Crohn's disease, celiac disease, atrophic gastritis, and pernicious anemia affect the gastrointestinal tract, potentially hindering the normal absorption process of this vital nutrient.
The absorption of vitamin B12 involves a complex process in the gastrointestinal tract. Understanding this mechanism is crucial to grasp how gastrointestinal disorders can disrupt the absorption process. Normally, vitamin B12 binds to a protein in the stomach, and this complex is later absorbed in the small intestine. Gastrointestinal disorders may interfere with these steps, leading to malabsorption.
A deficiency in vitamin B12 can manifest in various ways, affecting both physical and neurological health. Common symptoms include fatigue, weakness, anemia, and tingling sensations in extremities. Neurological symptoms may include difficulty concentrating, memory loss, and mood disturbances. Recognizing these signs is crucial for early detection and prompt intervention.
Healthcare professionals employ several diagnostic tools to assess vitamin B12 levels in individuals. Blood tests, specifically measuring serum B12 levels and other related markers, help determine deficiency. Additionally, intrinsic factor antibody tests and imaging studies may be utilized to identify underlying causes of malabsorption, such as pernicious anemia.
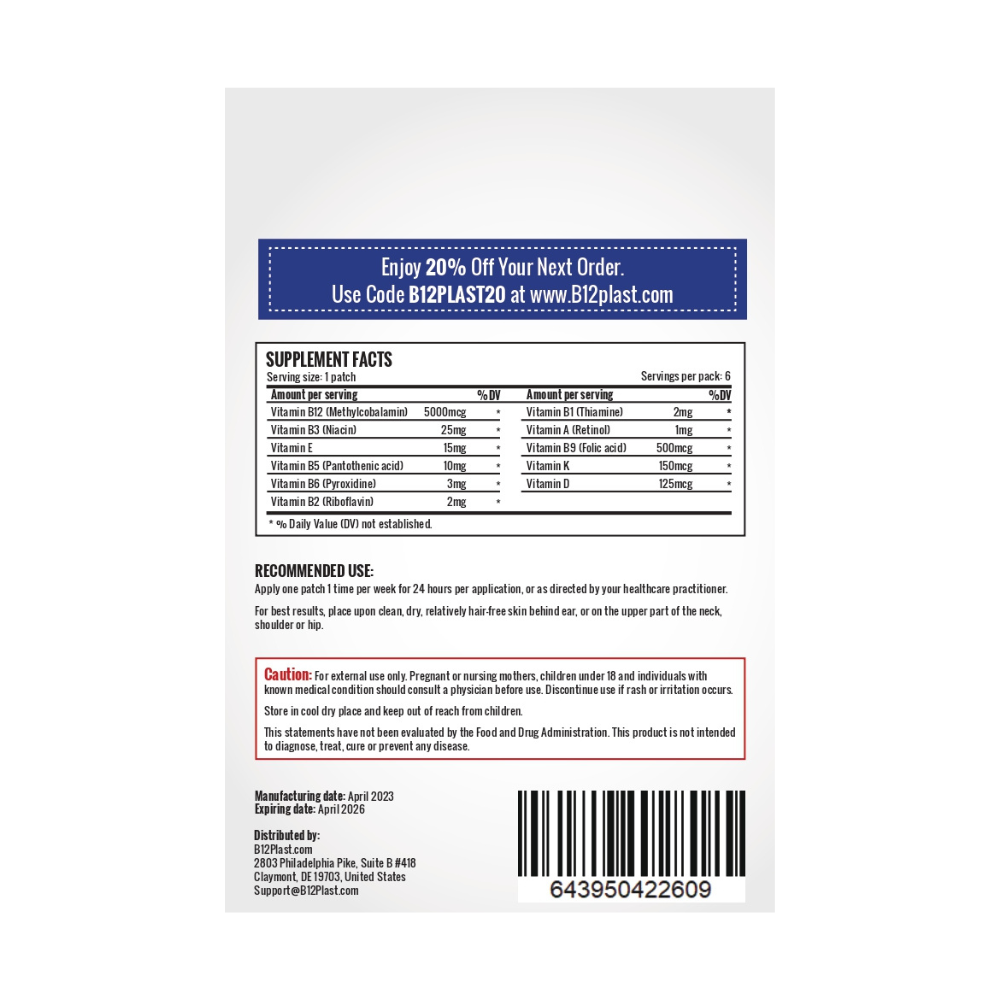
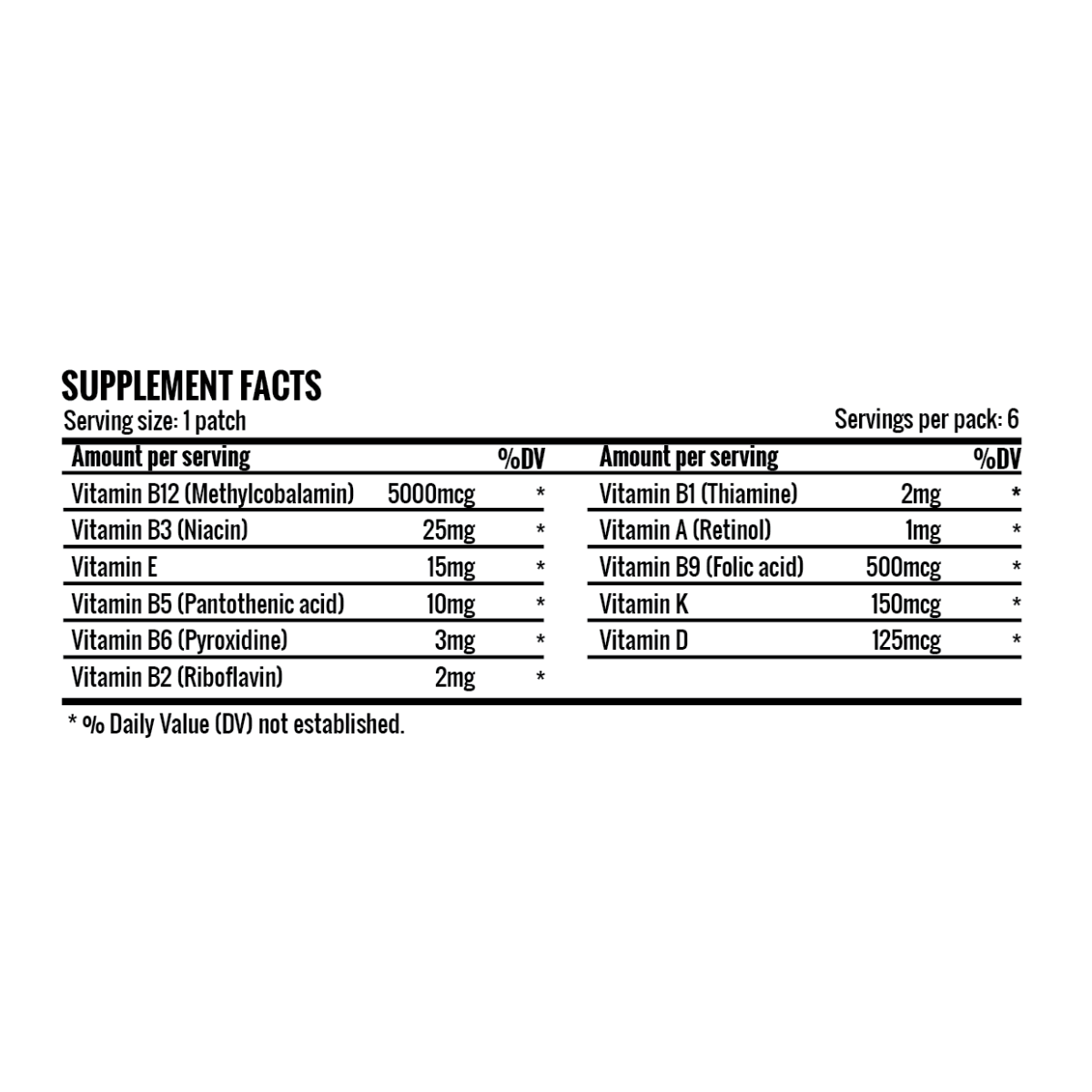
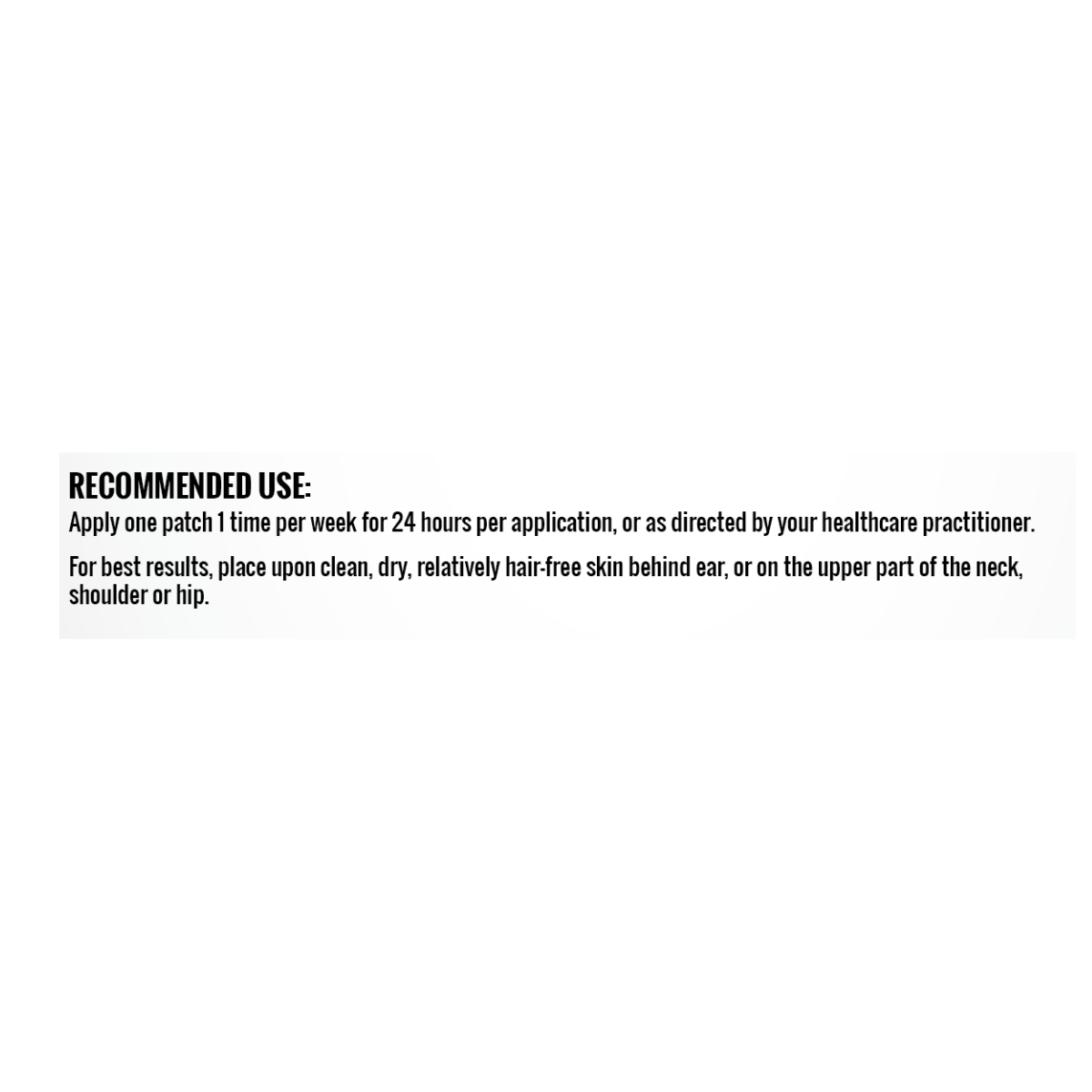
Treatment for vitamin B12 deficiency typically involves addressing the underlying cause while replenishing B12 levels. In cases of malabsorption due to gastrointestinal disorders, healthcare providers may recommend dietary modifications, oral supplements, or, in severe cases, B12 injections. Close monitoring and follow-up assessments are essential to ensure effective treatment and optimal recovery.
For individuals with gastrointestinal disorders prone to vitamin B12 malabsorption, preventive measures are paramount. Adopting a well-balanced diet rich in B12-containing foods, considering supplements, and managing the underlying gastrointestinal condition can help prevent deficiencies. Regular consultations with healthcare providers are essential to tailor preventive strategies to individual needs.
Illustrating the challenges and successes of managing vitamin B12 deficiency through real-life examples adds a human touch to the article. Sharing case studies or personal stories of individuals navigating gastrointestinal disorders and B12 deficiency can provide valuable insights and inspire others facing similar situations.
In conclusion, understanding the intricate relationship between vitamin B12 and gastrointestinal disorders is vital for both healthcare professionals and individuals managing these conditions. Addressing malabsorption issues early, through proper diagnosis and targeted treatment, is key to preventing and managing vitamin B12 deficiency, ultimately promoting optimal health and well-being.